治疗效果的论文
糖尿病
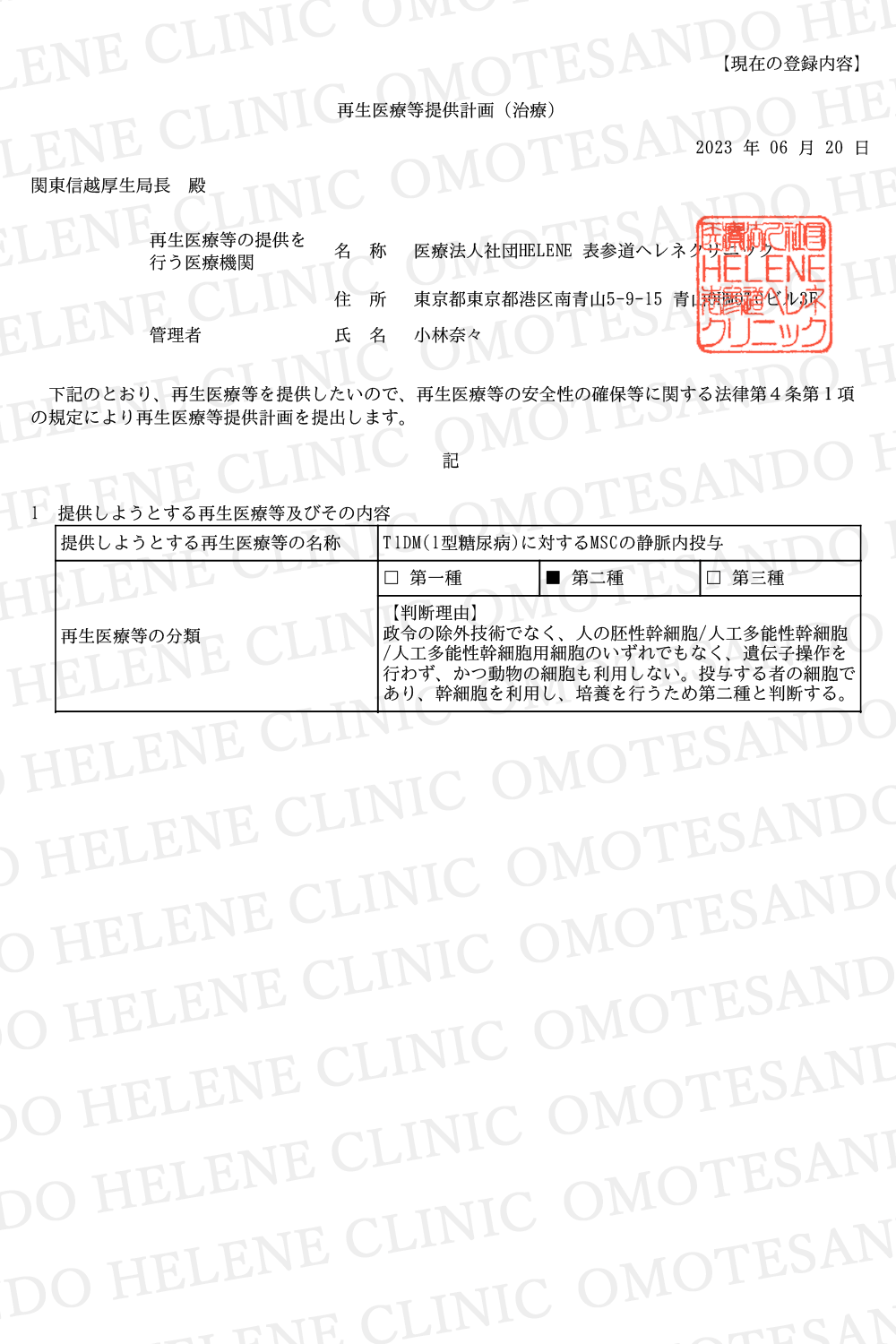
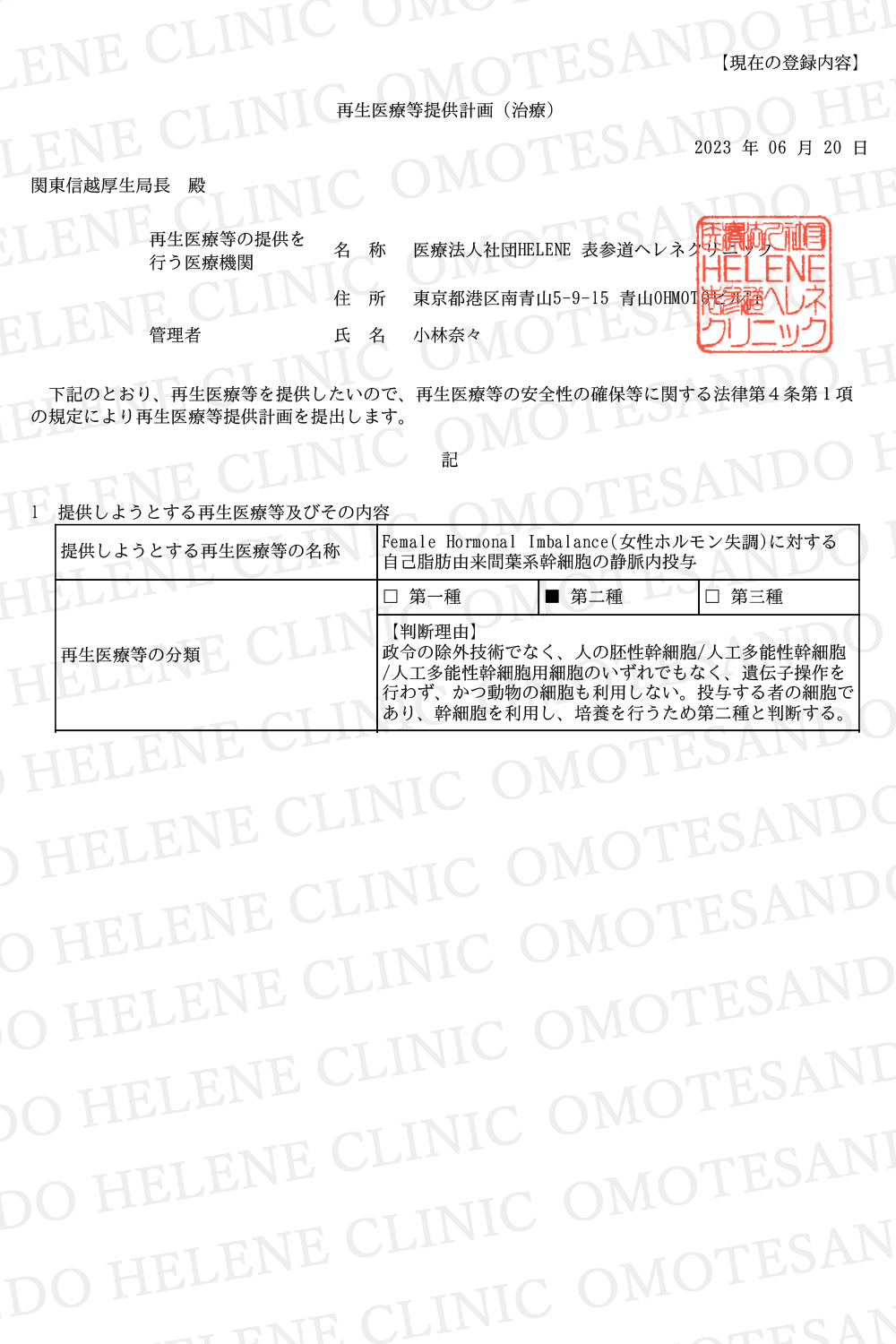
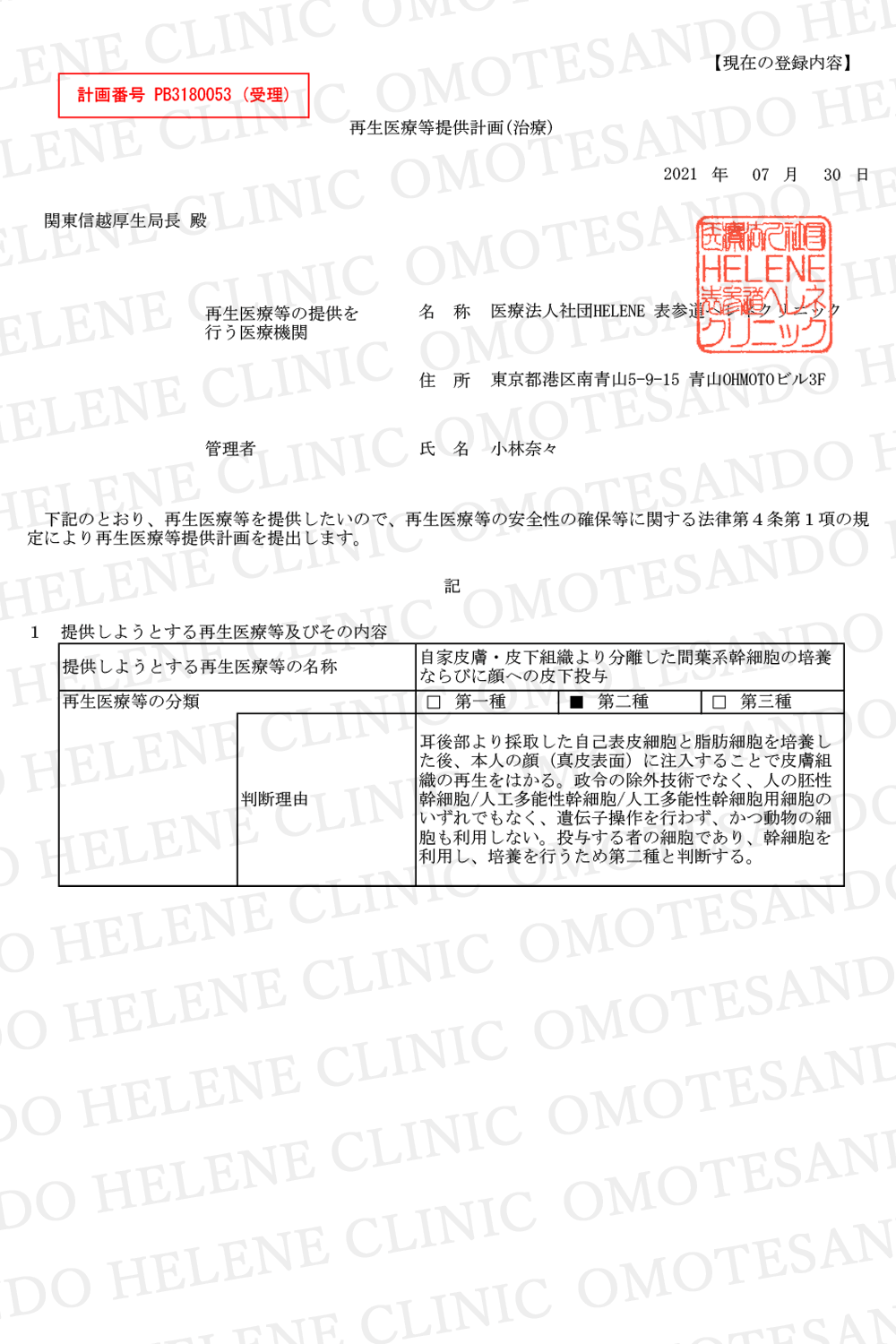
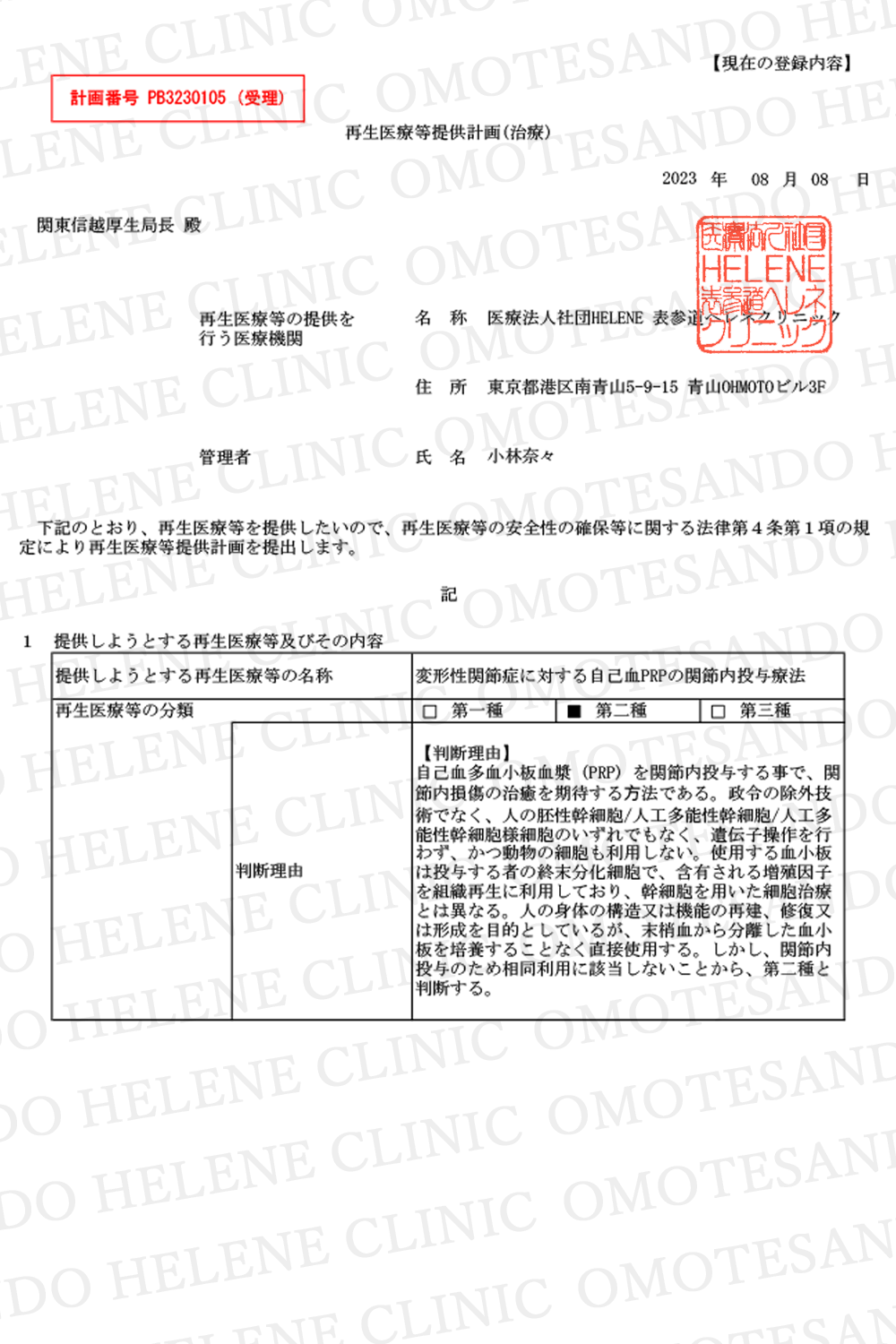
| Ref | Diagnosis Number of Cases – Age (Duration of T2DM) | Follow up | Source -SC Type – Passage, dose, Route, Repeat, Interval | Other T2DM Related Therapy | T2DM Related Outcome |
| 20 | T2DM1 56 (T), 62 (C) 18-60 y (T=8.6 ± 6.5, C=7.3 ± 6.3) |
1-2-3 mo, every 3 mo until -36 mo | T: Auto BM-MNC Dose ? DPA, 1x C: ( – ) |
T: D, E, PST, BGM-MA C: D, E, PST, IIT, BGM-MA |
HbA1c and C peptide in treatment were significantly better than either pre-therapy values or control. In Treatment: 18/56 patients insulin was discontinued; 19/56 insulin reduction > 50%, 10/56 insulin reduction 15-50%, 9/56 –non responder In control: 40/62 patients – insulin requirement increased > 50%, 22/62 patients – increased 15-45%. |
| 21 | T2DM 20 (MNC-HBO), 20 (MNC), 20 (C1=HBO), 20 (C2) 40-65 y (2 – 15 y) |
3-6-9-12 mo | Auto BM-MNC T1: MNC-HBO= 3641.2 ± 1585.4 M T2: MNC= 4012.5 ± 1431.9M DPA – 10 minutes 1x |
T and C: D, L, PST, SBGM- IA | Insulin dose reduction at 12 mo in T1 and T2, C1, C2 – unchanged Insulin free: T1: 1/20, T2: 2/20 Improvement at 12 mo in AUC C-Pep of T1= T2 > C1, and AUC Ins of T1 and T2. HbA1c at 3, 6, 9 and 12 mo -reduced significantly both in T1 and T2, but stable in C1 and C2. FBG at 6, 9 and 12 months – T1 and T2 -reduced Fasting C peptide at 3, 6, 9 and 12 mo significantly elevated in T1 and T2, but remained stable in C1 and C2 |
| 22 | T2DM 11 (T), 10 (C) T=46.5–56 y (10-15.5 y) C= 52.5–56 y (16-21 y) |
2-4-6-8-10- 12wk-4-5-6- 9-12 mo | T: auto BM- MNC – 290 M (220 -380 M) C: sham, saline SP/DA -1x after 12 wk: PB- GCSF- leucopheresis MNC – 490 (290–730M) C: sham, saline –IV-1x |
T and C: D, L, E, W-SBGM – IA | 12 mo: 50% Insulin reduction -Tr: 9/11 = 82%, -C:0/10, p= 0.002 Insulin red Tr > C (p=0.001, 6 mo), (p=0.004, 12 mo) HbA1C maintenance ( <7%): Tr 10/11 (91%), C 6/10 (60%), p= 0.167 |
| 23 | T2DM 10 (MSC), 10 (MNC), 10 (C) MSC= 36-58 (8-23) MNC= 39.5-50 (8.5-15) C= 43-59 (9-15) |
2-4-8-12- wk-6-9-12 mo | AutoBM-MSC-P4-5 – 1M/ kg BW Auto BM-MNC – 1B/patient C= vit. B complex SPDA – 1x |
T and C: L, PST,D-SBGM- IA | 6/10 (MSC), 6/10 (MNC), 0/10 (C) achieved primary end point: 50% insulin requirement reduction, while maintaining HbA1c
<7.0% -> significant difference |
| 24 | T2DM 31 (T), 30(C) 18-60 y (T=8.93±5.67 C=8.3±6.07) |
36 mo | T: Wharton jelly MSC P4 1M/kg BW C: Saline IV – 2x (interval 4 wk) |
T and C: D, E, PST, SBGM- MA | Blood glucose, HbA1c, Cpeptide, homeostasis model assessment of pancreatic islet cell function signifi- cantly improved- compared to control. Incidence of diabetic complications: Tr – no increase vs baseline, C: 4/30- new diabetic retinopathy, 3/30 new diabetic neuropathy 3/30 new diabetic nephropathy –> statistically significant difference (Tr vs C, P= 0.007) Insulin dose reduction: Tr: 18/31- 50% insulin dose reduction ( where 10/31 – insulin free from 311 mo postWJMSC, and insulin free duration 12.5±6.8 months),5/31 -1550% reduction, and 8/31 non responder Control: 14/30: >50% insulin dose increase, 16/30: 1545% insulin dose increase – 30/30 – non responder |
| 25 | T2DM + impotence2 7 (T), 3 (C) 57-87 (12-52 y, impo- tence minimal 6 months) |
2wk – 11 mo | T: UCB SC -His tos- tem, ABO, HLA- ABC, DR, and sex- matched – 15M C: saline Injection – CC -1x |
T and C:PST, D-SBGM-MA | Tr: Blood glucose levels decreased by 2 weeks, and medication dosages were reduced for 4 to 7 months (6/7). HbA1c levels improved after treatment for up to 3 to 4 months (7/7) Reduced insulin dose after 1 month (2/7) Control: no improvement in blood glucose level, HbA1c, and insulin dose. |
| 26 | T2DM 3 15 (T1), 15 (T2), 15 (T3), 3×5 C) T1= 57.7±8.2y (10.8± 7.3y ) T2= 55.3±11.4y (10.2± 5.7y) T3= 57.2 ±6.6y (9.6±4.5y) C= 58.7 ±7.3y (9.8±6.7y) |
12 wk 2y post study |
MPC- P(?) Rexleme- strocel-L – mesoblas Inc, cryo-thawed T1=0.3 M/kg T2=1 M/kg T3=2 M/kg C= placebo IV- 45 minutes 1X |
T and C: L, PST, BGM-RT | Tr: HbA1c – reduced – at all time points after week 1, C: a small increase in HbA1c Clinical target HbA1c <7% was achieved by 0/15 of Control, 2/15 of T1, 1/15 of T2, and 5/15 of T3 (P < 0.05) |
| 27 | T2DM4 13 (T), 13 (C) 10-58 y (0.5 – 11 y) |
1y | Hu fetal liver HSC – 35-55 M (20% CD34)- cryo-thawed Saline (C) IV – 1x |
T and C: BGM-FU | Up to 1 y, no significant improvement in fasting blood glucose, and C peptide compared to control. Improvement in – HbA1c only at 6th mo: 7.9±1.3 in treatment vs 7.0 ± 0.86 in control (p=0.046). None of the treatment become insulin free |
Ref= reference number, T2DM= Type 2 diabetes mellitus, treatment control allocation: 1 patient option, 2 successive: 2 Treatment – 1 Control, others: random, 3single blind multi center (18 –USA), 4=T2DM and T1DM, T= treatment, C= control, y= year(s), MNC= mononuclear cell, HBO= hyperbaric oxygen, MSC= mesenchymal stem cell, mo= month(s), wk= week(s)
SC= stem cell, Auto= autologous, BM= bone marrow, ?= data not available, DPA= dorsal pancreatic artery/substitute, M= million, SP/DA= superior pancreatic or duodenal artery, PB= peripheral blood, GCSF= granulocyte colony stimulating factor, IV- intra venous, P= passage, BW= body weight, B= billion, vit.= vitamin, SPDA= superior pancreaticoduode- nal artery, UCB= umbilical cord blood, CC= corpora cavernosa (penile root clamped with a band 30 min), MPC= mesenchymal progenitor cell, cryo= cryopreserved, hu= human, HSC= haematopoeitic stem cell, cryo= cryopreserved,D= diet, E= exercise, PST= previous standard therapy, BGM = blood glucose monitoring, MA= medication adjustment, IIT= insulin intensification therapy, L= lifestyle, SGBM= self blood glucose monitoring, IA= insulin adjustment, W-SGBM= weekly SGBM, D-SGBM= daily SGBM (minimum 5 points/week), RT= rescue therapy using oral anti diabetic agent, except thiazolidinediones in case there was unacceptable hyperglycemia, FU= at follow up
Current Stem Cell Research & Therapy, 2018(13)
Towards Standardized Stem Cell Therapy in Type 2 Diabetes Mellitus: A Systematic Review
Jeanne Adiwinata Pawitan, Zheng Yang, Ying Nan Wu and Eng Hin Lee
[20]Hu J, Li C, Wang L, et al. Long term effects of the implantation of autologous bone marrow mononuclear cells for type 2 diabetes mellitus. Endocr J 2012; 59(11): 1031-9.
[21] Wu Z, Cai J, Chen J, et al. Autologous bone marrow mononuclear cell infusion and hyperbaric oxygen therapy in type 2 diabetes mel- litus: an open-label, randomized controlled clinical trial. Cytother- apy 2014; 16: 258-65
[22] Bhansali A, Asokumar P, Walia R, et al. Efficacy and safety of autologous bone marrow-derived stem cell transplantation in pa- tients with type 2 diabetes mellitus: a randomized placebo- controlled study. Cell Transplant 2014; 23(9): 1075-85.
[23] Bhansali A, Upreti V, Khandelwal N, et al. Efficacy of autologous bone marrow-derived stem cell transplantation in patients with type 2 diabetes mellitus. Stem Cells Dev 2009; 18(10): 1407-16.
[24] Hu J, Wang Y, Gong H, et al. Long term effect and safety of whar- ton’s jelly-derived mesenchymal stem cells on type 2 diabetes. Ex- perimental and Therapeutic Medicine 2016; 12 (3): 1857-66.
[25] Bahk JY, Jung JH, Han H, Min SK, Lee YS. Treatment of diabetic impotence with umbilical cord blood stem cell intracavernosal transplant: preliminary report of 7 cases. Exp Clin Transplant 2010; 8(2): 150-60.
[26] Skyler JS, Fonseca VA, Segal KR, et al. Allogeneic mesenchymal precursor cells in type 2 diabetes: A randomized, placebo- controlled, dose-escalation safety and tolerability pilot study. Dia- betes Care 2015; 38(9): 1742-9.
[27] Ghodsi M, Heshmat R, Amoli M, et al. The effect of fetal liver- derived cell suspension allotransplantation on patients with diabe- tes: first year of follow-up. Acta Med Iran 2012; 50(8): 541-6.